 Professor Alain Maertens de Noordhout, 62, has been the Head of the Neurology department at CHR de Citadelle for the past 20 years and is specialised in movement disorders including Parkinson’s Disease. An expert in Deep Brain Stimulation, Professor Maertens also heads up the Human Neurophysiology Research Laboratory for Abnormal Movement and Headaches, teaches neurology, is chairman of the Scientific Committee of the Parkinson’s Association, serves on several expert panels and is associate editor of Acta Neurologica Belgica.
Professor Alain Maertens de Noordhout, 62, has been the Head of the Neurology department at CHR de Citadelle for the past 20 years and is specialised in movement disorders including Parkinson’s Disease. An expert in Deep Brain Stimulation, Professor Maertens also heads up the Human Neurophysiology Research Laboratory for Abnormal Movement and Headaches, teaches neurology, is chairman of the Scientific Committee of the Parkinson’s Association, serves on several expert panels and is associate editor of Acta Neurologica Belgica.
A proud father and grandfather, Professor Maertens enjoys fishing, tennis and walking in the woods around his home. He has a strict rule: no cellphones at mealtimes and believes in the importance of truly disconnecting.
1. Why did you become interested in Parkinson’s Disease?
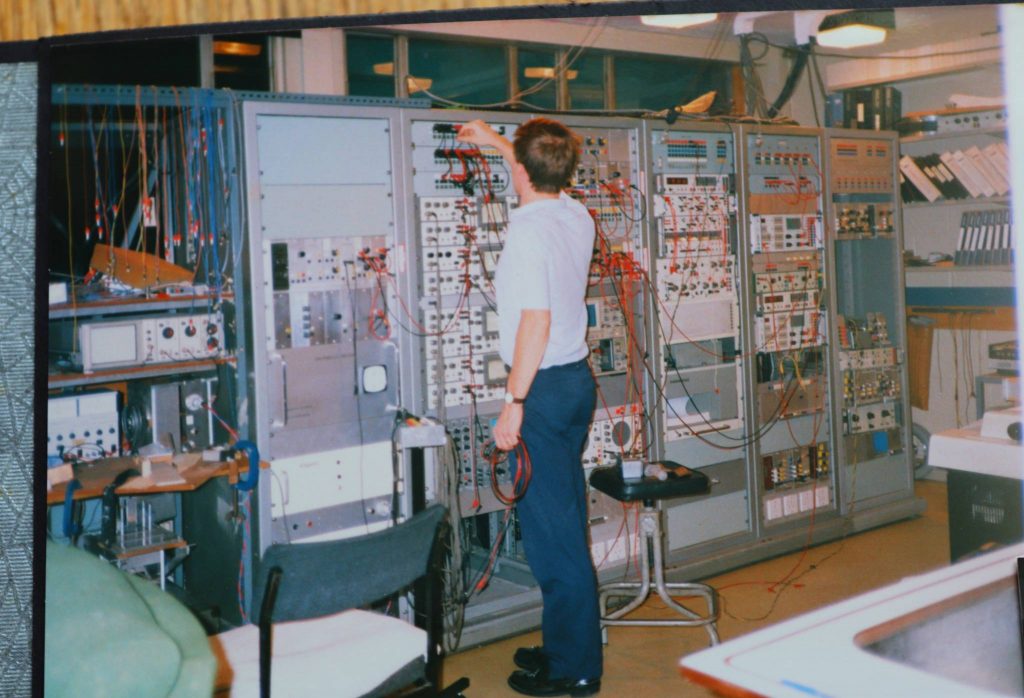 It was purely by chance, really. I got an opportunity to spend a year in the lab of (British neurologist) C.D. Marsden, who was kind of the ‘pope’ of neurology in the 1980s, and I was there at the time that embryonic cells were implanted into the brains of patients in the hopes of producing dopamine … which they did. But because they did not have the structures to connect them to the rest of the brain … they produced too much and had to be destroyed. (Photo: Professor Maertens in C.D. Marsden’s laboratory)
It was purely by chance, really. I got an opportunity to spend a year in the lab of (British neurologist) C.D. Marsden, who was kind of the ‘pope’ of neurology in the 1980s, and I was there at the time that embryonic cells were implanted into the brains of patients in the hopes of producing dopamine … which they did. But because they did not have the structures to connect them to the rest of the brain … they produced too much and had to be destroyed. (Photo: Professor Maertens in C.D. Marsden’s laboratory)
Nowadays, research teams hope to use stem cells which can both produce dopamine and create structures of control within the brain so they do not produce dopamine to excess. It will be 10-15 years more before this is available as a treatment but I saw the first two patients implanted in Sweden and then tested in C.D. Marsden’s lab as well as patients with very particular movement disorders, so this was the moment that I was hooked.
2. Why do you go to work each day? What gets you out of bed?
There is so little that is understood about Parkinson’s Disease and other movement disorders. We don’t know, for example, why some people get dementia and some people are particularly prone to falls. We still have so much to find out and to do in order to improve the lives of those with these conditions. I also have a commitment to my patients. I try to follow those that I see from early on all the way through their treatment. Some patients I have seen for 30 years.
3. What is patients’ most frequent initial reaction to their diagnosis? And what do you do/say to help them digest the news?
Shock. The announcement of the diagnosis is quite devastating to patients as this disease has a bad reputation. Just on Monday, I gave the diagnosis to a 41-year old man. It was a huge shock to him and to his spouse. People have an image in their mind of the late Pope John Paul II who was devastated by the disease, but he did not take all his medication as he should. He chose not to.
The important first step is to ensure that the person accepts the diagnosis and the fact that they will need to take medication for their rest of their life, but this is also true for those who have diabetes or hypertension. And then it is important for them to know that they are not the only one with this disease and there are associations to help support them.
4. What are the key pieces of advice that you give patients to help them manage in their daily lives with the disease?
We encourage them to do more sport. To do physio. If they do everything (as we prescribe), they have a good chance of living a good life, not as a sprinter but perhaps a marathon runner. We need them to feel optimistic and positive.
5. What is the role of family and friends in supporting patients?
Educating and supporting the family and caregivers is just as important. Because sometimes patients can be slow and it can be difficult or boring for the family to wait. But I always say, if it takes five minutes for them to do up a button, let them do it. They need time rather than too much help.
It is though exhausting for the family and there are groups in patient organisations to support them and also to ensure they feel connected and know what to do. For caregivers especially, it is important that they know, for example, that the drugs need to be delivered at a very particular time to be effective.
I encourage the spouse to come to the appointments with the patient and will ask them as well whether they have noticed any changes. They have a different perspective. Sometimes the patient does not want to mention something – like falling asleep during a meal, hypersexuality or a urinary infection, for example – but if I speak to the spouse separately from the patient then they will mention it. Or, for example, they might say that the patient is having delusions, or making a great deal of compulsive purchases online, or being very physical in bed when asleep, which will indicate to me that the patients’ medication needs to be tweaked. It is important to remain contactable for the patients as well as the spouses and caregivers.
 6. What do you wish you had known as a young doctor that you know now?
6. What do you wish you had known as a young doctor that you know now?
The importance of understanding the psychology of the patient. We have a few lessons in psychology as medical students but often the professor is boring … or mad … and our attention is elsewhere. But real psychology of the patient … really understanding what is important to them, to recognise changes and to know how to approach subjects … that comes with experience. It’s really important to ask the right questions at the right time.
(Photo: Professor Maertens holding a snake he caught in his garden!)
7. What future treatment option are you watching with most interest and hope?
There are some early signs of the disease that appear years before – such as losing their sense of smell and moving a lot in bed while asleep – and 80% of these people go on to develop and be diagnosed with Parkinson’s disease 10 to 15 years later. Researchers are working on understanding the mechanisms of the disease so that we understand why these are early indicators and then develop neuroprotective drugs so patients can avoid losing dopamine-producing cells. We don’t want people to panic if they have these symptoms but once we have a potential neuro-protective drug, we will need to screen people and enrol them in clinical studies. We will also want to screen people for genetic forms of the disease.
8. Which research avenue to find a potential cure excites you most?
Acting on alphasynuclein build up in the brain has a lot of potential. It has been shown that the protein unfolds into particular shapes that cannot then be evacuated by brain cells as it should be, which in turn causes the dopamine-producing cells to die. Once we know the process by which the protein unfolds, we could silence the abnormal genes so it can not unfold and accumulate.
9. What do you think the chances are that scientists will discover a cure in the next five, 10, 15 years?
Only a small proportion of cases are caused by genetics but I am pretty sure that in the next five to 10 years, we will have the first clinical trials for some of the genetic forms of Parkinson’s Disease for which we understand the sequence of the transformation.
Also in five to 10 years, we will want people to be coming forward to get screened to pick up early signs of the disease in order to join clinical trials for neuroprotective drugs.
10. What more needs to be done to speed up the development of effective treatments and, most significantly, a cure?
Of course, we need more funding for research. It is as simple as that. And we also need more money for associations to support the patients, families and caregivers. Education is vital.
11. What, if anything, gives you hope?
Until two years ago, children with spinal muscular atrophy would be devastated by the disease from their first birthday and pass away. Now that we understand what causes the condition, we have been able to develop a cure. The genetic mutation can be detected at birth and those children are treated so that they do not develop the disease. It is unbelievable. A miracle really. The same could happen for Parkinson’s Disease. Once we better understand the mechanism then we have a better chance to act.
12. What life lessons, if any, have Parkinson’s Disease patients and their loved ones shown/taught you? Has any particular patient inspired you and why?
I would say that I have learned to not always be in a hurry. To take the time. Of course, we don’t always have a lot of time, but we have to try to find ways to be available. To keep the dialogue going. The second life lesson/advice I have learned is humility. Some of my patients have become … well … almost friends. You make a commitment to them. The hardest part is when a patient doesn’t want to live anymore. In Belgium, euthanasia is allowed and Parkinson’s Disease is one of the conditions for which it is accepted. When a patient asks me to do that, it is very difficult. After years of treating them, they ask me to be there at the end. We are educated to cure people, not to kill them. And yet, if the patient wants you do it and a confidence has been built up over the years, it is their last request. This is very humbling and difficult.
13. What motto do you try to live by?
This is something that is important to me and I really believe in but I still have to get better at:
“Listen first, speak second.” And also … “Whatever you choose to do, do it to the best of your ability.”
(Photo: Professor Maertens de Noordhout teaching his granddaughter to fish.)

